Instructions on Utilizing Annual Physical Examination
Filling out the Annual Physical Examination form is a straightforward process that helps ensure a comprehensive health assessment. Once you’ve completed the form, it will contribute to a smoother and more efficient medical appointment. Please follow the steps below to fill out the form accurately and completely.
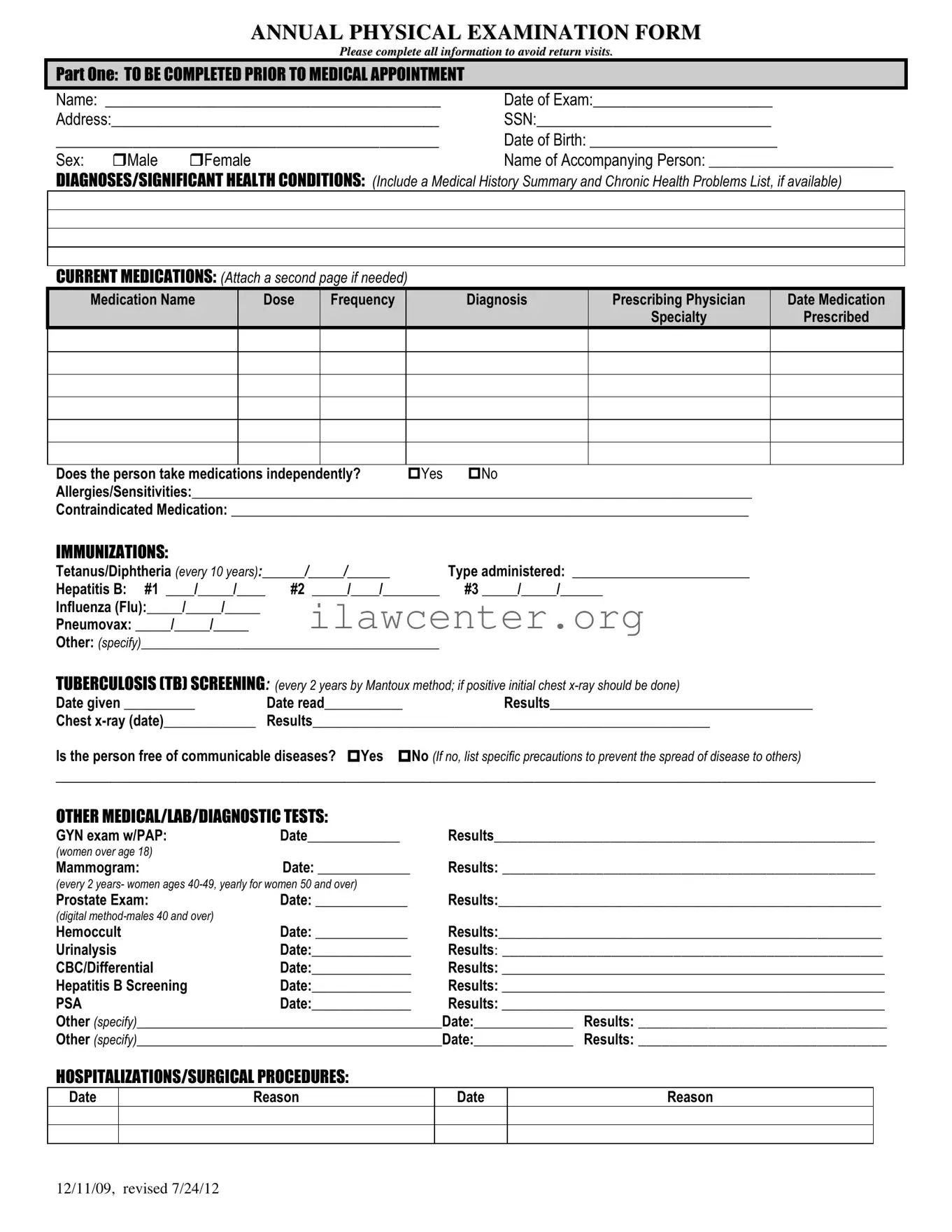
- Begin with Part One. Write your full name on the first line labeled "Name."
- Fill in the "Date of Exam" section with the date you are visiting the doctor.
- Provide your address including street address, city, state, and ZIP code.
- Enter your Social Security Number (SSN).
- Fill in your date of birth and select your gender by marking either "Male" or "Female."
- If someone is accompanying you, write their name in the designated spot for the "Name of Accompanying Person."
- In the section for Diagnoses/Significant Health Conditions, summarize your medical history and chronic health problems. Attach additional pages if necessary.
- List all current medications, including the medication name, dosage, frequency, diagnosis, prescribing physician, and the date prescribed. Attach another page if needed.
- Indicate if you take medications independently by selecting "Yes" or "No."
- Detail any allergies/sensitivities you have.
- Note any contraindicated medications if applicable.
- Fill in the Immunizations section with dates and types for Tetanus/Diphtheria, Hepatitis B, Influenza, Pneumovax, and any others as applicable.
- In the Tuberculosis (TB) Screening section, enter the date administered, date read, and the results.
- Answer whether you are free of communicable diseases by selecting "Yes" or "No." If "No," specify necessary precautions.
- In the section labeled Other Medical/Lab/Diagnostic Tests, document any relevant tests and results with corresponding dates.
- Finally, make records of any hospitalizations/surgical procedures by entering the dates and reasons in the provided spaces.
Once you have completed Part One, proceed to Part Two, which includes the General Physical Examination section. This allows for vital statistics and evaluations of various system functions. After filling everything out thoroughly, ensure all information is correct before submitting it to your healthcare provider.
- Input your Blood Pressure, Pulse, Respirations, Temperature, Height, and Weight in the respective fields.
- For the Evaluation of Systems, indicate "Yes" or "No" for normal findings for each system listed. Provide comments or descriptions if necessary.
- Complete the Vision Screening and Hearing Screening sections by selecting "Yes" or "No." Indicate if further evaluation is recommended by a specialist.
- Add any Additional Comments relevant to your medical history summary.
- Document any changes to medications or special considerations in the appropriate spaces.
- List any recommendations for health maintenance, special instructions, or dietary needs.
- Note any limitations or restrictions for activities and if you use adaptive equipment.
- Indicate if there has been a change in health status compared to the previous year.
- Clearly state if a recommendation for ICF/ID level of care is needed, along with any specialty consults.
- If applicable, note if a seizure disorder is present and the date of the last seizure.
Ensure the physician's name, signature, date, address, and phone number are provided before submitting the form. Having all sections filled out accurately contributes to better healthcare outcomes during your appointment.