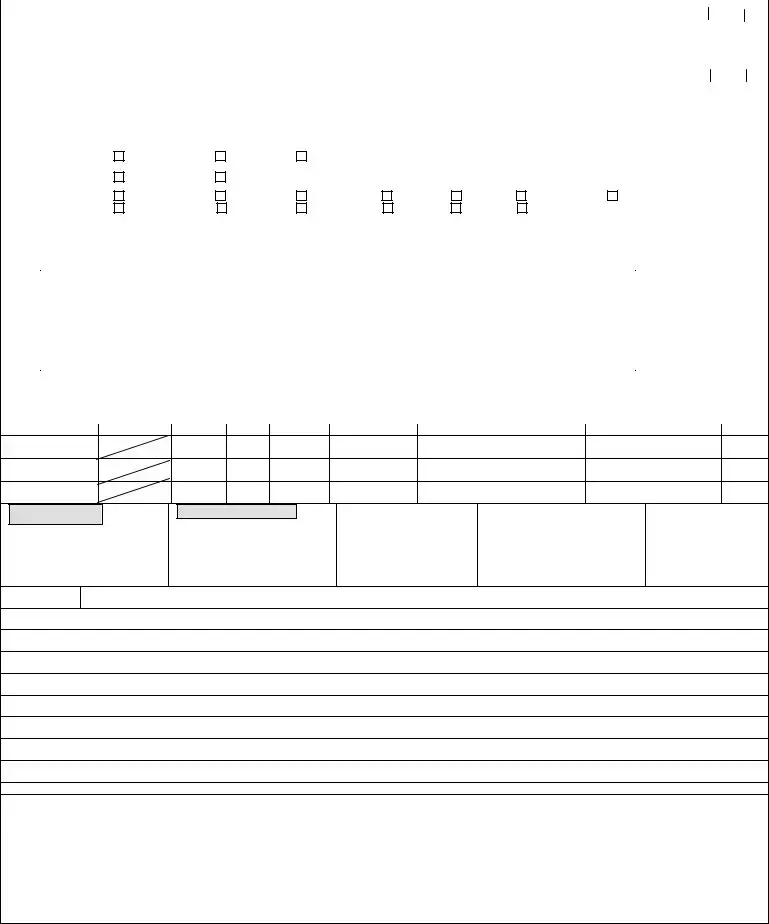
Instructions on Utilizing Patient Care Report
Completing the Patient Care Report form is essential for documenting medical responses and ensuring accurate patient records. Follow the steps outlined below to fill out the form correctly.
- Start by entering the Service Name and Vehicle Number at the top of the form.
- Fill in the Service Number and Incident Number.
- Write today’s date in the designated field.
- Document the Incident Location where the patient was found.
- Record the Patient’s Last Name, First Name, and Middle Initial.
- Enter the Age and Gender of the patient.
- Provide the Date of Birth for the patient.
- Fill out the Patient Address, including the City, State, and ZIP Code.
- Document the Chief Complaint.
- Indicate if the patient takes any Medications, selects from options: None, Unknown, or Brought with Patient. If applicable, list medications.
- Record any known Allergies, choosing from: None, Unknown, or listing specifics if any exist.
- Fill in the Medical History including conditions such as Asthma, Diabetes, etc., by selecting the appropriate checkboxes.
- In the General Patient Care section, record vital signs like Blood Pressure, Respiration, and Temperature.
- Document treatments provided and specific Medications Given, including quantities and dosages.
- If applicable, obtain Patient Signature and the Date/Time of refusal of treatment/transport.
- Get signatures from witnesses and crew members, along with their EMS License Numbers.